Wake Up! Why Poor Sleep Could Be Killing You

By the time things got really bad, that period when Brandi Muridian would be too exhausted to make it through a day at work or get out of bed for an entire weekend, the 40-year-old wife and mother had been chronically under-slept for about a decade. Still, even after cutting back on caffeine, adopting earlier bedtimes, taking up exercise—even knowing that she snored and suffered night after night of inferior slumber—sleep disorder never crossed her mind.
“I just thought maybe it was stress,” she says. “Maybe it was anxiety or I wasn’t getting enough sleep, although I was sleeping a lot. I could sleep 10 to 12 hours, wake up and be so exhausted I’d go back to bed for another four to five hours for a nap. For a long time, I told people I’m just one of those people who needs a lot of sleep.”
It wasn’t until she was diagnosed with fibromyalgia and her rheumatologist’s insistence earlier this year that she get a sleep study as a way to minimize triggers for the condition – of which poor sleep is one – that she came eye to bleary eye with the true source of her problem.
“I honestly I didn’t think I had sleep apnea. I thought, ‘OK I snore a little,’ but I thought I was fine,” she says. “But I was willing to do whatever just to feel better because my life was awful.”

The Sleep You’re Not Getting
Americans have a problem with sleep, and not just the ones dealing with a diagnosed disorder. Somewhere along the line, as our nation careened to the never-unplugged, something’s-always-going-on cacophony it is today, we decided that to sleep is to miss something or to concede a step to the other guy. Society rewards those who are always on and never out of reach, plus our pioneering spirit framed prolonged wakefulness as just another manifestation of the unbreakable American will.
“There’s sort of a societal basis to pushing as hard as you can and not getting proper sleep,” says Clint Mickle, co-owner and executive director of Little Rock-based Sleep Management Services. “Some people just go ‘I don’t sleep good,’ but there’s more to it. There’s an underlying cause to why you’re not sleeping or, even if you are sleeping, why you’re not feeling restored and refreshed.”
The National Heart, Lung, and Blood Institute estimates 40 million Americans—about one in six—have some sort of sleep disorder; sleep apnea alone affects about 18 million adults, says the National Sleep Foundation. One in 10 of us has Restless Leg Syndrome, the involuntary “pins-and-needles” nerve activity that keeps us tossing. Other conditions are brought on by prolonged upheavals in one’s circadian rhythms, the natural internal clock that tells us when it’s time to wake and time to rest.
“There are a few genetic links to sleep disorders, but not that many, actually. A lot of them are acquired disorders,” says Dr. David Davila of Baptist Health Sleep Center in Little Rock. “Lack of sleep situations are either volitional, people intentionally curtailing their sleep opportunities in order to work longer or from family or social pressure, or they’re involuntary, they just get into situations that they can’t control and end up with short sleep periods.”
King among sleep disorders is sleep apnea, of which obstructive sleep apnea is the most common. Sleep apnea is an involuntary cessation of breathing that causes arousal and prohibits restorative sleep, particularly in the sleep stages where the body enjoys the most benefits. Apnea patients generally don’t awaken during such episodes, but are deprived from getting rest even if technically asleep.
“So what that does to you is you might be able to get enough hours of sleep, but it’s not good quality sleep, and you’re not rested and you are tired and fatigued in the morning,” says Dr. Khaled Khasawneh of the University of Arkansas for Medical Sciences Sleep Clinic in Little Rock. “What happens usually when you fall asleep is your muscles are more relaxed. People with normal muscle tone are able to keep their airways open, but people who are born with a genetic predisposition have abnormal muscle tone and their airways collapse at night and become obstructed.”
Risk Factors For Sleep Apnea
As a means of evaluating one’s risk for sleep apnea, Dr. Khaled Khasawneh suggests STOP BANG:
S |
Snoring |
T |
Tired during the day |
O |
Obstruction; someone has observed that you stop breathing while you sleep |
P |
Pressure; blood pressure high enough to require medication |
B |
BMI; greater than 35 |
A |
Age, risks go up after 50 |
N |
Neck circumference greater than 17 inches (male) or 16 inches (female). |
G |
Gender; men are more likely to suffer sleep apnea, particularly compared to premenopausal women. After menopause, incident rates level out. |
The Physical Repercussions
The effects can be devastating in one’s everyday life. Besides causing the sleep-deprived to be cranky and unable to concentrate during the day, some studies link lack of sleep to weight gain and a not-coincidental sapping of the energy one would otherwise expend at the gym.
“The biggest thing when it comes to rest and sleep and weight loss is that it affects my clients’ moods, and they don’t have the energy that they need to be able to push it and make progress,” says Tyler Lawrence of Fit Factory in Little Rock.
“When you’re going into a weight-loss program, we’re messing with your food. We’re changing what you intake. So whatever you would typically eat for energy, more than likely we’re going to be taking some of that away and your body has to adjust to that. If you’re not getting enough sleep, it just compounds on you, especially in the beginning.”
Difficulty in taking off pounds is just one part of the vicious cycle in which poor sleepers often find themselves. Sleep apnea is not genetic, but certain factors increase one’s likelihood of developing it— excessive weight being one of them—even in childhood.
“There are some people who have obstructive sleep apnea as kids, and that’s usually recognized early because parents watch their kids a lot and they see when they stop breathing,” says Khasawneh.
“If you have a genetic predisposition, like any other disease, there is a time in your life where this disease gets manifested. It can get manifested just on its own; that’s why we have a significant number of patients who have obstructive sleep apnea that aren’t overweight, they are not obese. You look at them and they look young and healthy and fit.”
Forget the Stereotypes
Daniel Moody is one such individual. The 26-year-old freelance photographer has displayed the classic symptoms of sleep apnea since he was a child.
“I know that this is very common, or at least it’s diagnosed, in people who are overweight and older, but I’ve had these experiences since I was young and I’ve always been fairly fit,” he says. “What seems most likely to me is that people are just kind of ashamed to do it. It just seems like a daunting task to go get a sleep study or it just seems like since you don’t fit the overall criteria, you just kind of doubt the probability of it.”
Moody, who describes his sleep apnea as “mild,” finally did a sleep study a few months ago and wasn’t surprised to learn of his condition. In fact, whatever effort it took to finally have the study was rewarded with a formal strategy for dealing with the condition and finding some relief.
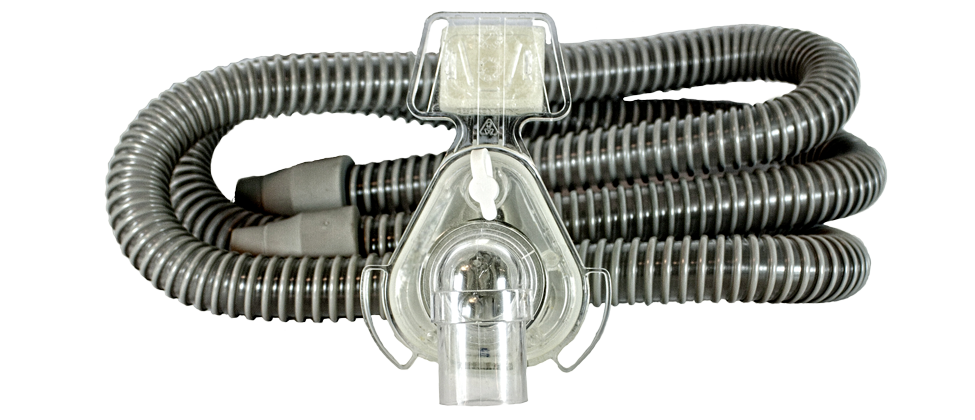
“The test itself can be a little challenging to rev up for; they do strap a whole bunch of stuff to you,” he says. “Once you’ve done it, it’s a little less daunting if you have to come back for a second one for a follow-up, which is very common so that they can see without the [Continuous Positive Air Pressure or CPAP] machine and with the machine.
“I’d probably say that it’s good for anybody to do [who] has any issues with sleeping because it might not be simply sleep apnea; there could be a number of other sleep disorders that can lead to it,” Moody says.
Whatever the circumstances, the cumulative impact of not getting enough sleep is serious. Over time, sleeplessness contributes to heart disease, diabetes and stroke. Even short-term sleep deprivation can have serious consequences, says Davila, who recently attended a conference on drowsy driving co-sponsored by the National Highway Safety Administration and the National Sleep Foundation.
“There’s a suspicion that possibly up to 20 percent of fatal accidents are related to drowsy driving—and that is grossly underestimated,” he says. “They’re trying to set some kind of standard for lack of sleep and driving; they’re saying if you haven’t slept two hours, you’re impaired. Most people would say you need more sleep than that to be a safe driver, but that was a guideline that came out.”

How’s Your “Sleep Hygiene”?
Sleep disorders aside, there are plenty of distractions and bad habits that cost us getting some good shut-eye. Here are the National Sleep Foundation’s tips for getting the seven to nine hours every adult should sleep every night:
- Stick to a sleep schedule, even on the weekends.
- Practice a relaxing bedtime ritual.
- Avoid naps, especially in the afternoon.
- Exercise daily, even light to moderately, at any time of day other than when you should be sleeping.
- Keep your bedroom cool—between 60 and 67 degrees—and free from noise and light.
- Sleep on a comfortable mattress and pillows. A mattress older than nine or 10 years has outlived its usefulness.
- Manage your circadian rhythms. Avoid bright light in the evening; expose yourself to sunlight in the morning.
- Avoid alcohol, cigarettes, caffeine and heavy meals in the evening.
- Wind down. Spend the last hour before bed doing a calming activity such as reading.
A Sleep Study May Help
One treatment option is the CPAP, a breathing device worn at night that assists in keeping airways open. Recent developments include a retainer-like device that moves the jaw into better alignment for breathing, as well as a more invasive procedure that stimulates the hypoglossal nerve in the tongue through electric impulse, much like a pacemaker for the heart. The proliferation of sleep labs, both in hospitals and in standalone businesses, provides multiple options for diagnosis, but consumers should know what to look for.
“The gold standard in the sleep testing industry is accreditation either by the American Academy of Sleep Medicine or the Joint Commission,” Mickle says. “Seeking treatment with a board-certified sleep medication physician is critical, although there’s not that many out there. In order to get testing, you don’t have to see a board-certified sleep medicine physician; your primary care specialist can get the ball rolling.
“If nothing else, people should consider having a sleep study for peace of mind. It’s one night out of your life to potentially impact your life in a huge way.”
Muridian, whose test revealed her apnea was interrupting her sleep up to 90 times an hour and whose subsequent treatment has brought her life back into balance, could not agree more.
“My quality of life is so much better and I wish I had done it years ago,” she says. “I feel like I missed out on all that energy and all of those things I could have done when I was lying in bed being exhausted.”

CENTRAL ARKANSAS SLEEP LABS
Restless to solve your sleep problems? Here are a few local sleep centers with experts who can help:
Baptist Health Sleep Center
9500 Kanis Road, Little Rock
501-202-1902
Sleep Disorders Center
Arkansas Children’s Hospital
1 Children’s Way, Little Rock
501-364-4000
Sleep Management Services
9305 Treasure Hill Road, Little Rock
501-224-5200
UAMS Sleep Clinic & Sleep Lab
11300 Financial Center Parkway
Suite 900, Little Rock
501-526-6090







